October 2021 – In this issue of Gibson Talks, Colleen Watford, Director of Executive Search at Gibson Consultants, and Andy De, Vice President of Go-to-Market Strategy and Marketing at MedeAnalytics, sat down to talk about Andy’s predictions for healthcare delivery. Looking into the future, Andy discusses the strategic implications of the digital transformation of healthcare that will change healthcare, clinical, and business processes through the embrace of innovative technologies.
Q: How will healthcare providers embrace a convergence of AI (Artificial Intelligence) and machine learning for spatial, predictive, and prescriptive analytics?
A: Providers will find opportunities with technology to design new facilities, optimize their supply chains, and forecast the most promising elective procedures.
There is a need to enable advanced predictive, prescriptive, and spatial analytics to empower executives, line of business (LOB) leaders, clinicians, and nurses at the point of care. This need is driving a convergence of AI (machine learning, deep learning, natural language processing) and descriptive and spatial analytics with actionable, forward-looking insights for critical decision-making.
Health systems and hospitals will leverage these advanced technologies and analytic process automation (APA) to:
- Locate new facilities, testing centers, and supply chain warehouses ensuring access and convenience for patients, their families, and caregivers as well as their constrained capacity for cardiovascular procedures, hip and knee replacements, cancer care, etc.
- Optimize their supply network especially for overseas suppliers, enable accurate and reliable demand forecasts and potentially work with emergency response inventory services providers (ERISPs) to ensure that they will not run out of N-95 masks, personal protective equipment (PPE), ventilators, testing equipment and supplies, critical therapeutics, and vaccines, as well as medical devices and equipment needed to treat patients while assuring the safety of healthcare personnel in the event of a pandemic or epidemic and the resulting surge.
- Leverage advanced analytics and AI to forecast demand for the elective procedures and services most in-demand from their patient population (leveraging clinical, financial, and socio-economic determinants of health data) which they have adequate capacity for, and which are also profitable for them to deliver from a revenue and margin perspective.
Q: How will visionary innovation leaders at leading healthcare organizations and health systems embrace medical robotics?
A: Medical robotics hold promise for enabling process automation as well as higher efficiencies while assuring safety for their healthcare personnel and front-line workers.
One of the most significant areas of the digital transformation of healthcare and its underlying clinical processes for patient engagement, diagnosis, and post-discharge patient care and recuperation is AI and analytics-enabled robotics, including enabling technologies like machine vision and exoskeletons.
Here is a strategy framework that articulates the four primary areas and 14 applications that are being/will be enabled by robotics in the post-pandemic “new normal,” many of which are already in use across the world at this time.
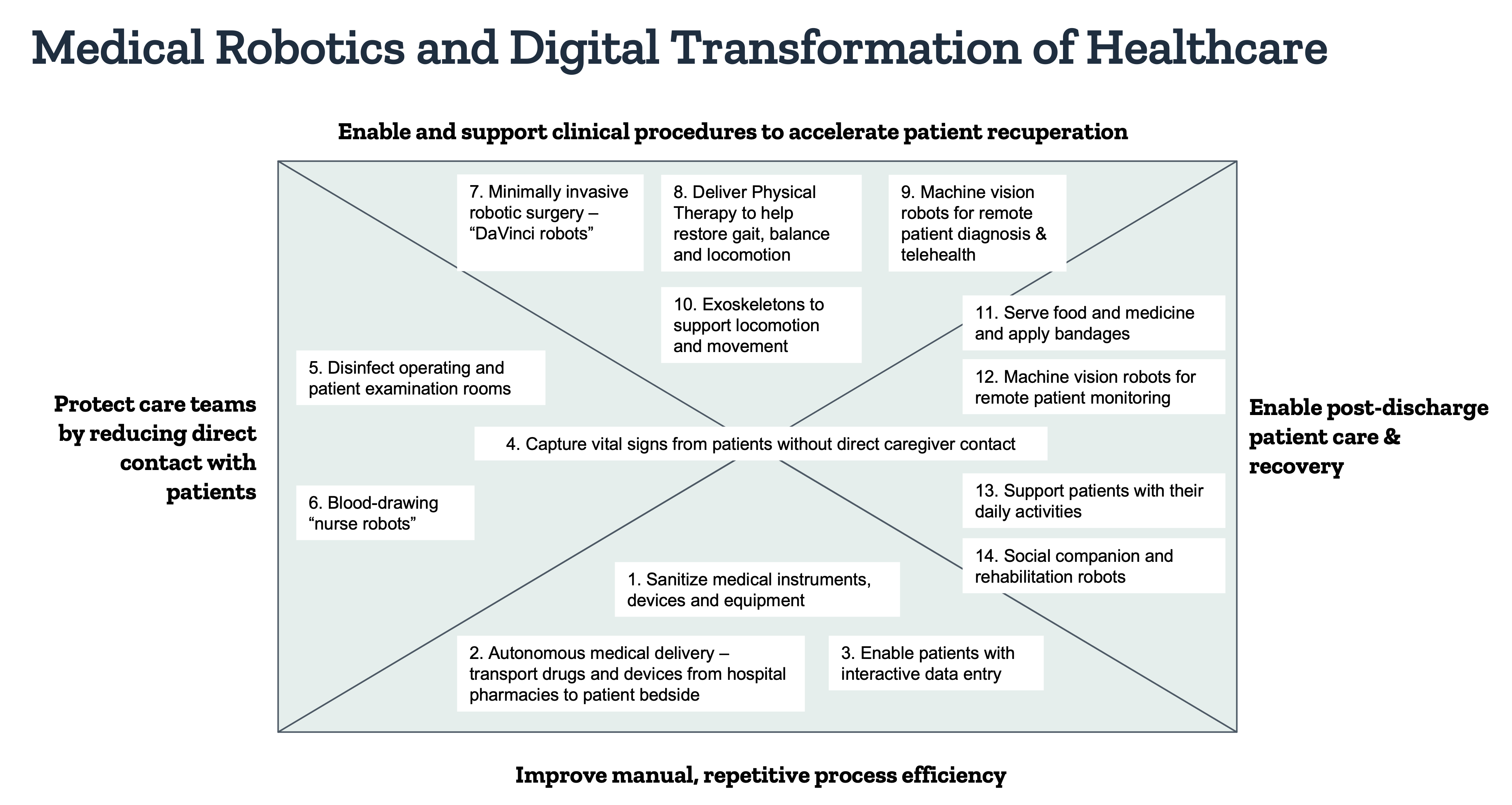
Figure 1. Strategy Framework articulating the deployment of medical robots in the post-pandemic “new normal.” Copyright Andy De (2020). All rights reserved.
The deployment of medical robots for multiple applications ranging from improvement of manual process efficiency to protection of care teams through non-contact diagnosis, enablement, and support of clinical procedures to enabling post-discharge patient care and recovery, is an idea that has already been tested in countries like Japan, China, South Korea, and Taiwan, and whose time has come.
Q: As payers embrace AI, analytics, and analytic process automation, what types of opportunities will it present to them?
A: Payers will be better positioned to protect revenue, segment, target and recruit new customers, minimize fraud waste and abuse, and improve process efficiencies.
2021 will be a challenging year for healthcare payers given 30 MM+ Americans who have lost their jobs and insurance coverage as well as 9 MM+ Americans who have been infected with COVID-19. Healthcare payers who are under tremendous cost pressures, as well as unprecedented changes to their reimbursement mixes (thanks to the explosive growth of telehealth and similar services), will extensively leverage advanced descriptive, spatial, predictive, and prescriptive analytics as well as analytic process automation (APA) to:
Figure 2. Strategy Framework potential high-value areas of investment in advanced analytics, AI, and analytic process automation (APA) from healthcare payers. Copyright Andy De (2020). All rights reserved.
(A) Innovate with New Products and Services for New Segments of Customers
The COVID-19 pandemic and the resulting economic catastrophe has resulted in 30+ MM Americans who have been laid off or furloughed with loss of employer-provided health coverage. At the same time, 9 MM+ Americans have been infected by COVID-19 and will likely suffer from its side-effects and after-effects, resulting in COVID-19 becoming a “pre-existing condition” for these affected patients. Deploying advanced analytics and AI will not only help payers identify the changing need of their customers, but also identify new prospects in the wake of the pandemic and respond to their evolving needs with newer products and services that will enable new revenue streams to compensate for lost revenue.
(B) Minimize Customer Churn thru Value-Added Programs
Advanced predictive and prescriptive analytics has already helped large healthcare payers like Aetna to better understand their customer behavior, dissonance with their products and services, and deploy value-added programs to minimize customer churn which have helped protect millions in revenue that would otherwise have been lost. Payers should continue to utilize this data to inform the development of programs to achieve customer goals.
(C) Improve Process Efficiencies
Healthcare payers are challenged with a number of administrative processes (e.g., claims administration and management) that are manual, inefficient, onerous, and negatively impact employee morale. Industry leaders will deploy best practices like data analytics and AI-enabled lean six-sigma for value stream mapping to stratify current processes in terms of value-added (VA) vs. non-value-added (NVA) process steps from the customer’s perspective. This will enable them to eliminate NVA processes or steps that will not only enhance process efficiency, customer satisfaction, and employee productivity but also millions in cost savings.
(D) Minimize Fraud, Waste and Abuse
Fraudulent claims filed on behalf of patients by unscrupulous physicians, providers, and predatory pharmacies are a significant challenge that costs healthcare payers billions in leakage every year. Deploying advanced machine learning and natural language processing (NLP) algorithms with analytic process automation (APA) is helping payers to proactively flag and detect fraud, waste, and abuse pertaining to claims administration, management, and reimbursement; and save them millions in leakage and cost savings each year.
About the Participants

Andy Dé is the Vice President of Marketing at MedeAnalytics, enabling the go-to-market strategy, planning, and execution with a focus on customer value and impact. Prior to joining MedeAnalytics, Andy has held strategy, marketing and product management leadership roles at SAP Health Sciences, GE Healthcare, Tableau and Alteryx where he helped grow their healthcare and life sciences business.
Dé is passionate about healthcare innovation and authors the Health Sciences Strategy Blog (www.HealthScienceStrategy.com) and its companion Twitter feed (@HITstrategy) with a readership audience across 47 countries. He has been quoted and published in leading healthcare publications including Healthcare IT News, Becker’s Hospital Review, Health Informatics, Modern Healthcare, Search Health IT, Health Data Management (HDM), Health Management Technology, Fierce Healthcare, Health IT Outcomes, Hospital and Health Networks and the Washington Post. He was recognized as one of the 2019 and 2018 HIMSS Social Media Ambassadors (SMAs) by the Healthcare Information Management Systems Society (HIMSS).
Andy holds masters’ degrees in engineering and business on scholarships from leading institutions in the USA, Canada and Israel. He has completed executive management programs on Artificial Intelligence (AI), Disruptive Innovation, and Health-Science Strategy from Harvard Business School (HBS), the Sloan School of Management at MIT, and the Kellogg School of Management, respectively. His professional profile can be accessed at www.andyde.com
 Colleen Watford is a Director of Executive Search at Gibson Consultants and specializes in recruiting for the Digital Health market. Colleen works with entrepreneurs and investors to help their companies scale by finding top leadership talent.
Colleen Watford is a Director of Executive Search at Gibson Consultants and specializes in recruiting for the Digital Health market. Colleen works with entrepreneurs and investors to help their companies scale by finding top leadership talent.



Leave a Reply